Colorectal cancer is a common disease. It is one of the most frequently diagnosed cancers in the world – ranking third behind lung cancer and liver cancer – and it affects almost as many women as men1.
Its incidence rate of colorectal cancer is particularly high in the United States, in certain South American countries, in Europe, in Australia and New Zealand, and more recently in Japan. In general, epidemiological studies reveal that socioeconomic status is an important prognostic factor for colorectal cancers, and that there is inequality between low income patients and those with higher incomes. A difference in exposure to risk factors (especially food), for example, could explain this inequality. In addition, low incomes, a low level of education, and insufficient health coverage would limit access to appropriate preventive, diagnostic, and therapeutic care for the less-favored patients. However, the main factor affecting survival at the time of diagnosis is the stage of the tumor.
3rd
Colorectal cancer is the third most widespread cancer in the world and the second for the most cancer-related deaths2.
930,000
Every year, nearly 930,0001 people die from colorectal cancer worldwide.
1.9M
There were nearly 1.91 million new cases of colorectal cancer around the world in 2020.
A progressive tumor
Colorectal cancer develops from a cell in the inner lining of the colon or rectum. This cell multiplies uncontrollably and gradually changes into a tumor, also known as a polyp. Polyps are growths that form in the inner wall of the colon, in the mucous membrane. The risk of a polyp turning into cancer varies, depending on the size of the benign tumor and type of cells.

A silent cancer
The absence of symptoms is common. Colorectal cancer can therefore develop silently and can remain undiagnosed for a while. This is why screening is necessary. Nevertheless, some signs may point to the need for consultation with your physicial (see below).
Age: main risk factor
Most of colorectal cancers occur in people over 50 years of age2. While some factors are genetic, others are preventable with a change of lifestyle. Regular exercise and a diet rich in fiber and fruits and vegetables are beneficial. Conversely, the risk of colorectal cancer is increased by a diet rich in red meat and cured meats, excess weight or obesity, excessive alcohol consumption, and smoking2.
Inflammatory bowel diseases (Crohn’s disease and ulcerative colitis) are also risk factors for colorectal cancer3.
Recognizing the signs
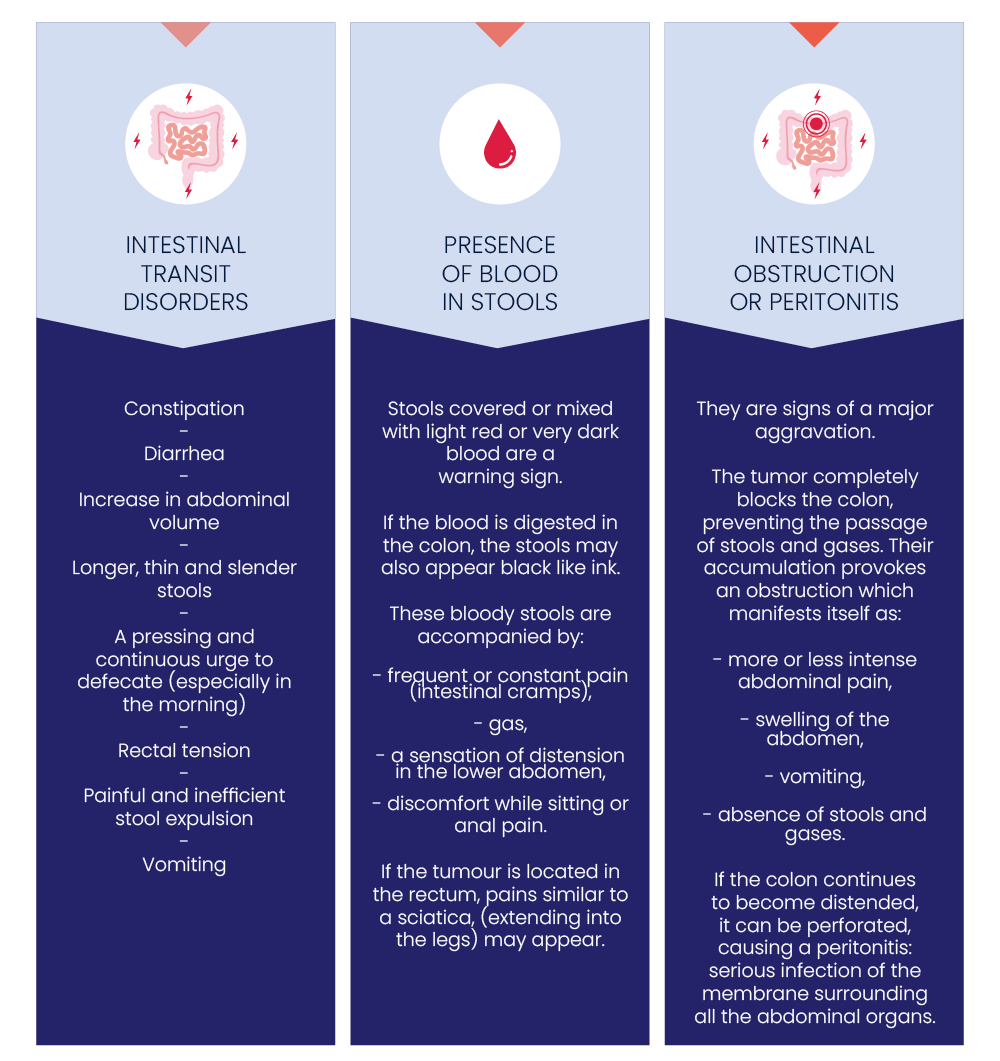
Illustrated infographic presenting the signs of colorectal cancer – Source: APHP – consulted in February 2024
Different types of therapeutic approaches
Different types of treatments can be prescribed for colorectal cancer, depending on the stage of the disease and the general condition of the patient. These include surgery, radiotherapy, chemotherapy, and targeted therapies. Depending on the case, a single treatment or a combination may be prescribed. These treatments can have different objectives depending on the stage of the disease: to remove the tumor through surgery, to use radiotherapy to stop it from spreading, or to improve the patient’s quality of life by minimizing their symptoms.
AND SERVIER?
Guided by the needs of patients, we aim to bring therapeutic innovations to the development of treatments targeting hard-to-treat cancers. Specifically, these include digestive cancers (colorectal cancer, gastric cancer, pancreatic cancer, cholangiocarcinoma, a rare and aggressive biliary tract cancer), glioma (brain tumors), hematologic cancers (acute myeloid leukemia, acute lymphoblastic leukemia, lymphomas) or pediatric cancers.
We are focusing our R&D programs on two approaches: immuno-oncology and targeted therapies.
In order to improve treatment of patients with colorectal cancer, Servier contributes to:

