At Servier, we are convinced that collaboration between public and private actors is a powerful tool to accelerate innovation and meet patient needs. Public-private partnerships (PPPs) are a unique collaborative model, making it possible to pool expertise and resources and share risks to accelerate the discovery and development of new therapeutic solutions. To this end, we are engaged in many international projects in all our therapeutic areas.
Définition
A PPP is based on contractual collaboration between different actors in the public sector (universities, hospitals, research institutes, etc.), the private sector, and patient associations. Together, they contribute their expertise to a public health project. As part of a long-term dynamic, these initiatives, lasting 3 to 10 years depending on the nature of the project, aim to accelerate the transformation of scientific discoveries into concrete solutions for patients.
1. Accelerating healthcare innovation through collaborative dynamics
In a world where scientific and technological advances are progressing at lightning speed and unmet medical needs require innovative and personalized approaches, PPPs offer a unique framework for accelerating therapeutic innovation.
PPPs help to remove certain scientific and technological barriers by pooling expertise to bring innovative solutions to patients faster. For instance, the sharing of knowledge between scientific experts, physicians and industry accelerates the transition from basic research to clinical applications.
2. Maximizing the probability of success by sharing risks
PPP funding predominantly relies on public or institutional funds, which makes it possible to support ambitious research projects, sometimes perceived as too risky for exclusively public or private funding.
This secure environment encourages pharmaceutical companies to invest in areas where progress remains to be explored and thus increases the probability of success for their research projects.
These collaborative initiatives, like those of the Innovative Health Initiative (IHI) program, help break down traditional barriers by providing a cooperative space that is conducive to innovation.
3. Meeting patient needs by pooling resources and expertise
The complexity of clinical studies, the ever-increasing regulatory requirements and the challenges associated with industrialization represent long, expensive and risky processes for healthcare actors, requiring considerable resources and multidisciplinary expertise.
PPPs, by their collaborative nature, allow the generation of large databases (chemical libraries, clinical-biological data, epidemiological data, etc.) and access to expensive infrastructure such as biobanks, new preclinical models, or new technologies and specialized equipment. For example, thanks to the amount of data generated, this pooling of resources makes it possible to identify sub-populations of patients for a given disease and thus provide personalized care, meaning the ability to provide the right treatment to the right patient.
These large-scale projects make it possible to deal with health challenges that are too ambitious for a single actor to tackle alone – such as rare diseases and the integration of health data – transforming competitors into collaborators.
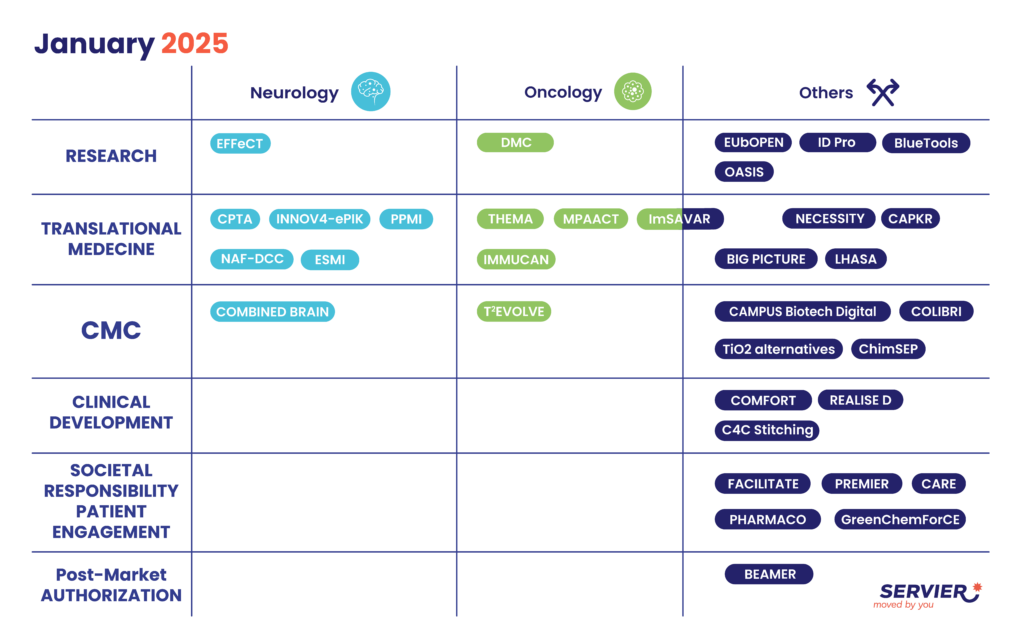
We actively participate in nearly forty PPPs in France and abroad (Europe, the United States, Canada, the United Kingdom, Australia, etc.). Our contributions take various forms, such as providing our in-house expertise, robust data, new technologies and/or funding, each with a unique objective: to solve a common public health problem that would be impossible to achieve alone. Our expertise, along with our long-term vision enabled by our unique governance model, serves as a true differentiating factor alongside our partners, while involving the patient at every stage. Public-private partnerships contribute positively to development and performance and fully illustrate the Group’s ambition to adopt a collaborative approach that is a catalyst for innovation.
Nathalie de Préville, Director of Public-Private Partnerships, Servier
34
As of January 2025, Servier is engaged in 34 PPPs across 35 countries. Around 150 employees and 300 external partners contribute to the PPPs in which we are involved
