Chronic venous disease (CVD) is a global phenomenon1. According to Vein Consult, almost 84% of adult patients show at least one clinically observable sign of CVD, ranging in severity from simple functional symptoms to the most severe injuries.
Chronic venous disease: a silent condition
A disease that evolves in a variety of ways
The term chronic venous disease (CVD) encompasses all clinical manifestations of venous system dysfunction in the lower extremities. This progressive disorder, characterized by valvular insufficiency, venous obstruction or both, leads to venous hypertension that manifests in different ways, from simple telangiectasias (small, dilated superficial vessels) to active venous ulcers.
Classifications of CVD
Specialists in CVD rely on the CEAP categorization (Clinical, Etiological, Anatomical, Pathophysiological), which differentiates among seven stages in the disease’s progress. The scale ranges from C0, characterized by no visible signs, to C6, corresponding to an active venous ulcer, and serves as an objective metric of the disease’s evolution2:
Once it reaches the C2 stage, the disease is generally considered progressive and requires specialist medical supervision. This stage often marks the beginning of a treatment process that can be lengthy and complex for patients.
About half the patients examined in the Vein Consult program have moderate to severe forms (C2 to C6).
Increasing prevalence
Given the aging population and the rise in obesity worldwide, the prevalence of these diseases continues to grow.
The Vein Consult program has revealed a striking regional contrast: the early stages of the disease are predominant in every region. The proportion of early stages of the disease is higher in the Middle East and Asia, while the share of advanced stages is higher in Central and Eastern Europe and Latin America.
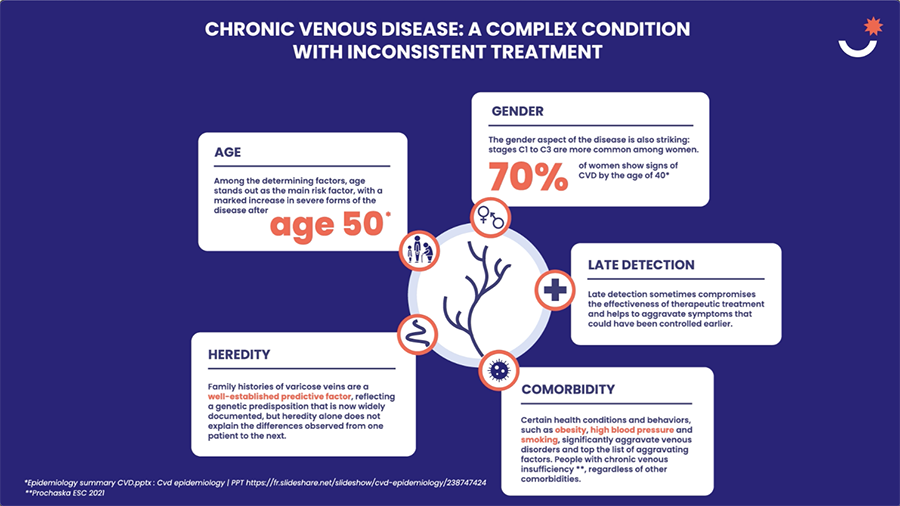
Multiple and complex risk factors
Inconsistent treatment
Multifaceted symptoms that complicate diagnosis
The diverse clinical manifestations of chronic venous disease poses a real challenge for healthcare personnel. Feelings of heaviness, varicose veins, pain, pruritus, cramps…: the range of symptoms, often diffuse and nonspecific, makes early identification particularly complex. This is especially true insofar as symptoms do not always correlate with the severity of the venous condition.4
If there are no obvious signs, symptoms can easily be underestimated by patients and healthcare professionals alike. This standardized approach often delays diagnosis, prolongs the diagnostic odyssey and allows the disease to progress, whereas earlier treatment could reduce its impact.
A treatment process fraught with pitfalls
The pathway of individuals with chronic venous disease reflects the complexity of treating the illness. Diagnosis is often made at a symptomatic stage, because specialists are often enlisted only when varicose veins appear.
A study presented at a recent meeting of the International Union of Phlebology shows that more than half of patients in some areas of the world have never been seen by a medical professional for venous symptoms.5
“A disease that is both widespread and underestimated calls for a paradigm shift. Chronic venous diseases must now be recognized as a true public health priority. Their close link with cardiovascular disease and their major impact on patient quality of life amply justify this reassessment.”
What can be done to improve treatment?
Raising awareness: an essential proactive step
In the face of a silent disease, better information about early signs, risk factors and possible consequences of CVD is critical. Incorporating venous prevention into awareness-raising campaigns aimed at the general public and healthcare personnel would enhance global consciousness of the disease.
Early diagnosis: key to effective management
Detecting CVD before the onset of advanced forms of the disease would help prevent complications and steer patients more rapidly toward appropriate treatment. Patients are strongly motivated to consult their physician, but physicians must also be trained to identify symptoms in a timely fashion – through the use of medical questionnaires, for example, so as to identify at-risk individuals and refer patients to specialists more efficiently.
A standardized clinical assessment might be a solution as well. The systematic use of diagnostic tools would not only allow for earlier detection but also guide patients more effectively on their treatment path.
A healthy lifestyle: Prevention for better control
Some aggravating factors for CVD, such as sedentary habits, overweight or smoking, can be managed with appropriate changes in lifestyle. Regular physical activity, such as walking or swimming, along with weight control, a balanced diet and cessation of smoking are among the various options available to patients for preventing the onset or progression of the disease. Therapeutic patient education plays a key role in empowering patients faced with CVD.
[1] Epidemiology of chronic venous disorders in geographically diverse populations: results from the Vein Consult Program – PubMed – https://pubmed.ncbi.nlm.nih.gov/22466974/
[2] Medipedia (https://medipedia.be/fr/insuffisance-veineuse/symptomes/les-differents-stades-de-linsuffisance-veineuse
[3] Les stades de l’insuffisance veineuse – Paris Veine Institut – https://www.veine-institut.paris/stades-insuffisance-veineuse/#:~:text=Le%20stade%20C0%20%3A%20aucun%20signe,l%27examen%20de%20la%20jambe.
[4] SLR CVD_Int Angiol-4877_Epub_V1_2022-03-18
[5] https://www.revue-phlebologie.org/donnees/portedocument/mes_telechargements2.php?cparam=55017hxtxwbxs4j3cljgfxsdh2g7hvkhvntn3awuo2sy3hftp71x0qjo058marz : mes_telechargements2.php
